How to Fix System Thermal Solution Compromised
Abstract
Teeth that require endodontic treatment are often structurally compromised and this considerably complicates endodontic procedures. Therefore, pre-endodontic restoration is a key approach that dentists should consider for such teeth. This article discusses current concepts of pre-endodontic restoration, with a focus on adhesive restorative methods and surgical/orthodontic techniques, and provides a relevant decision-making flowchart.
Key points
-
Highlights the importance of pre-endodontic restoration for the predictability of endodontic treatment.
-
Discusses restorability aspects for structurally compromised teeth.
-
Reviews current restorative and surgical/orthodontic techniques for pre-endodontic restoration and provides a decision-making flowchart.
Introduction
The purpose of endodontic treatment is to prevent or treat apical periodontitis by maintaining an aseptic root canal system or disinfecting this when previously infected.1 Rubber dam isolation of the subject tooth is considered mandatory as it prevents ingress of oral bacteria and saliva, precludes inhalation and ingestion of instruments, and averts leaking of irrigation solutions into the oral cavity.1
Teeth that require endodontic intervention are often structurally compromised due to conditions such as caries, trauma, or root resorption. The limited residual tooth tissue substantially complicates endodontic procedures. Considering pre-endodontic restoration before initiating endodontic treatment is valuable for compromised teeth as this approach:
-
Simplifies optimal rubber dam isolation for the subsequent endodontic visits2
-
Creates space for prolonged function of irrigation solutions3
-
Allows for effective inter-appointment temporisation to prevent bacterial microleakage, seepage of intracanal medicaments and gingival ingrowth into the cavity4
-
Prevents fractures of the weakened tooth structure, thus maintaining repeatable reference points5
-
Improves aesthetics during the endodontic treatment period, thus enhancing patients' acceptance
-
Facilitates post-endodontic restoration.
While traditional non-adhesive techniques of pre-endodontic restoration, such as amalgam core build-up, copper bands or temporary crowns, may still prove useful for some clinicians when appropriately performed,6 they also present with many shortcomings which, along with the development of adhesive approaches, have limited their clinical value for this purpose.7 , 8 These techniques will not be further considered in this article but the reader may refer to Table 1 for a brief overview.
Full size table
The aim of this article is to provide an evidence-based overview of modern concepts of pre-endodontic restoration focusing on restorative techniques with bondable materials and surgical/orthodontic techniques that expose tooth tissue.
Restorability considerations
Restorability assessment is essential before embarking on endodontic treatment. This should include evaluation of the restorative status of the tooth (structural, periodontal, endodontic), as will be discussed in the following sections, although local and general factors relating to the context of treatment (for example, tooth used as an abutment for fixed or removable prostheses, parafunction, medical history, patient expectations, cost) should also be examined.9
Certain restorability indices9 , 10 have been developed to aid decision-making by quantifying clinical judgements; however, their validity is not sufficiently tested and subjective elements are still included.
Structural assessment
Clinicians should be cognisant that typical clinical and radiographic examination may have limited sensitivity in detection of caries, cracks and marginal deficiencies.11 Therefore, definitive assessment of restorability should be performed only after total removal of previous restorations, caries and unsupported tooth tissue.
The importance of a circumferential 1.5-2 mm band of healthy tooth tissue, namely ferrule effect, is well established for a positive prognosis, yet current evidence suggests that presence of a partial ferrule (1-3 walls) may be sufficient.12
Other biomechanical parameters, such as residual cusp thickness and loss of marginal ridges, also need to be assessed as these have been shown to impact on tooth stiffness.13 Besides, fracture resistance can be enhanced by preserving pericervical dentine through conservative access cavity preparation.14
Periodontal considerations
Another consideration is the potential infringement of deeply subgingival restoration margins within the supracrestal tissue attachment (STA),15 formerly known as biologic width, which consists of the junctional epithelium and supracrestal connective tissue attachment. STA violation is believed to trigger adverse periodontal effects, although the specific aetiology (biofilm, trauma, material toxicity, combination of factors) is not clear.15 Mean STA apico-coronal dimension is found to be 2.15-2.30 mm; however, considerable variability exists according to tooth type, site, periodontal health and healing time after previous surgery.16 Thus it would be prudent not to rely on mean values but to attempt measuring the STA dimension at each individual situation. A simple method is by transgingival probing, which is considered comparably reliable to direct bone sounding after flap reflection,17 although it might be influenced by probing force18 and the inflammatory state of the tissues.19 Other researchers suggest accounting for the full supracrestal gingival tissue (including gingival sulcus) to address variations in sulcus depth.20
Many other factors (Box 1), such as having a favourable crown-to-root ratio (up to 1:1)21 and width of keratinised tissues (≥3 mm),22 may influence restorability as well as the technique selection for pre-endodontic restoration (Fig. 1).
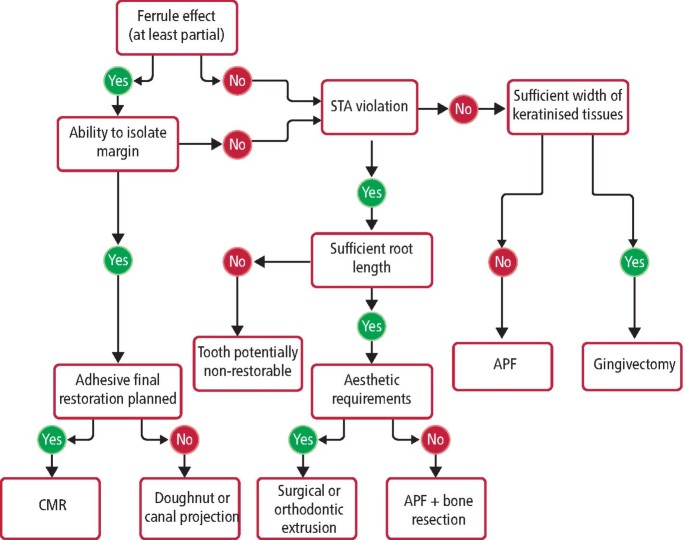
Decision-making flowchart for pre-endodontic restoration
Full size image
Endodontic considerations
Clinicians should also assess whether the subject tooth is amenable to endodontic treatment (primary, secondary or surgical). This requires evaluation of several parameters, such as the presence and extent of periapical pathology, root damage (fractures, resorption, perforation), complexities in root canal system (obliteration, separated instruments) and proximity to adjacent anatomical structures.9
Planning final restoration
Following restorability assessment, it is crucial that the definitive restoration of the tooth is decided at this early stage as this could also influence the technique selection for pre-endodontic restoration (Fig. 1). In addition, when a cuspal coverage final restoration is planned, cusp reduction may be performed at pre-endodontic stage to improve visibility and protect the tooth from fractures.5
Restorative techniques
According to the above, a pre-endodontic restorative technique is indicated for teeth with at least partial ferrule as well as cavity margins that enable moisture control and do not infringe into the STA (Fig. 1). A summary of current methods, using materials that can bond to tooth tissue, is provided in the following sections.
Cervical margin relocation
Relocating a deep cervical margin to a supragingival position using resin composite was first described by Dietschi and Spreafico23 as 'cervical margin relocation' (CMR). Other researchers have termed this technique as 'deep margin elevation'24 or 'proximal box elevation'.25
This approach is highly indicated when an adhesive final restoration is planned;24 for example, in case of a localised deep margin where the remaining walls provide sufficient enamel for bonding (Fig. 2). More specifically, it allows for immediate dentine sealing (IDS) to be performed in freshly cut dentine just before relocating the margin and this prevents dentine contamination, enables bond maturation and enhances bond strength of the subsequent indirect restoration.26 A second IDS can be performed after completion of endodontic treatment to provide an immediate seal of the root canal obturation and optimise the cavity for the indirect restoration by blocking undercuts.24 Moreover, the supragingival location of the margin aids the subsequent procedures of impression taking and final cementation.24

Cervical margin relocation (CMR): from pre-endodontic to post-endodontic restoration. a) Non-vital upper right first molar after removal of caries and previous restorations. b) Isolation and c) mesial CMR with sectional matrix. d) Pre-endodontic restoration (including cusp reduction) completed. e) Preparation for adhesive restoration after completion of endodontic treatment. f) Ceramic onlay after adhesive cementation
Full size image
The main limitation of CMR is that adequate seal of the margin with a well-fitted matrix under rubber dam isolation is considered as a necessary prerequisite,24 although this is not always achievable, especially for subgingival margins. In addition, sufficient coronal walls should be remaining in order to support the matrix,24 which can be reduced at thin sections so as to be able to slide subgingivally and provide a tight seal. Stabilisation of the matrix can be achieved by packing of polytetrafluoroethylene (PTFE) tape (as wedging is usually not feasible) or by the double matrix technique (a sectional matrix inside a circumferential matrix) in deep localised cavities.24
CMR has been described with either packable or flowable composite, which have shown comparable marginal integrity in vitro.27 Marginal adaptation can be optimised by placement of packable composite in small increments rather than a single layer,25 decreasing its viscosity through pre-heating28 and limiting the overall thickness of flowable composite to 1-1.5 mm due to its higher shrinkage and lower filler content.29
Doughnut technique
Different approaches may be considered when a non-adhesive final restoration is planned (for example, conventional crown); for example, in teeth with multiple missing walls and a large amount of peripheral margin into dentine. In these situations, matrix stability is usually not achievable,24 and free-hand30 or two-step (free-hand followed by secondary placement of matrix)31 pre-endodontic core build-ups may be applied as an interim solution to facilitate endodontic treatment before definitive crown preparation (Fig. 3).
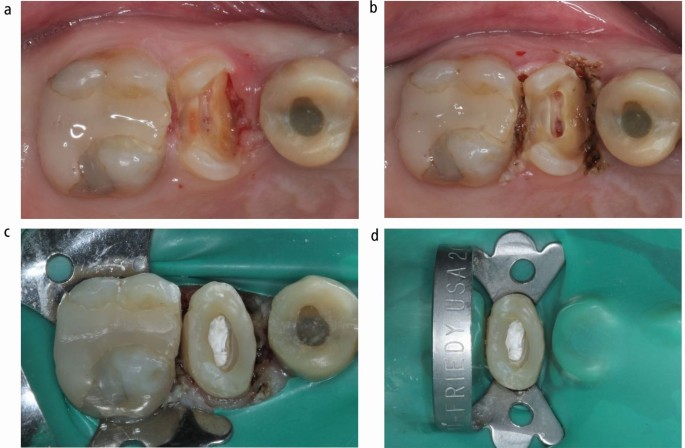
Combined pre-endodontic restoration of an upper right second premolar. a) Pre-operative condition with subgingival mesial and distal margins. b) Following laser gingivectomy. c) 'Doughnut' composite build-up using polytetrafluoroethylene in pulp chamber. d) Final rubber dam isolation before initiating endodontic treatment
Full size image
The so-called 'doughnut' technique involves a circumferential build-up of the cavity walls and use of a suitable barrier (cotton pellet, thermoplastic gutta-percha, PTFE, liquid dam) to prevent blockage of root canal orifices (Fig. 3c). This method is mainly described with free-hand flowable composite build-up after using retraction cord in the sulcus to displace the soft tissues.3 , 30
Advantages include the relatively simple application and the maintenance of access to the root canal system that prevents complications in canal location and patency.30 Concerns arise regarding marginal adaptation and management of overhangs, especially when applied free-hand, although it could be argued that the cervical proportion of the material will be removed during the subsequent crown preparation to natural tooth tissue margins.
Following completion of endodontic treatment, and before proceeding to the final composite build-up of the 'doughnut' cavity, clinicians may consider fibre reinforcement of the peripheral walls to enhance the stress-absorbing capacity of the core.32
Canal projection
As an alternative to the above technique, this approach involves core build-up with projection of root canal orifices from the pulp chamber floor to the cavosurface.33 Canal projection provides better visualisation and straight-line access to the canals, canal individualisation in case of close proximity of canal orifices on the chamber floor, correction of misdirected access cavity and enhanced hydraulic condensation of obturation materials as well as adequate sealing and reinforcement of the chamber floor or perforation repair materials.2 , 33
This technique has been described with the dedicated Projector Endodontic Instrument Guidance System (PEIGS; CJM Engineering, USA), which consists of a tapered plastic device sliding onto an endodontic instrument to preserve canal patency.33 Alternative methods, including use of hypodermic needles34 or Greater Taper gutta-percha points (Fig. 4),2 , 3 are easily accessible, more affordable and offer equivalent results.2 , 3
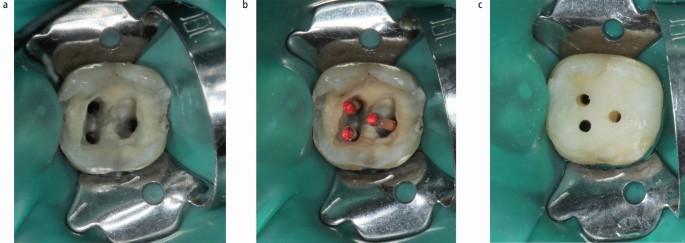
Canal projection on a lower left second molar. a) Access (after removing caries/previous restorations) and flaring of coronal third of root canals. b) Greater taper gutta-percha points to preserve canal patency. c) Finalised pre-endodontic composite build-up with projected root canals to the cavosurface
Full size image
A relevant drawback compared to the 'doughnut' might be the more time-consuming procedure for the build-up as well as for the temporisation between endodontic visits, as each projected canal needs to be temporised as a separate cavity.
A modification of this method can also be applied for pre-endodontic restoration of cervical lesions with pulp involvement, such as extensive Class V cavities3 or external cervical resorption,35 in order to maintain patency to the root canal system.
Open-sandwich technique
This technique is mainly described with an intermediate layer of resin-modified glass-ionomer cement (RMGIC) as a base for overlying composite build-up.36 It has been advocated due to the advantages of using glass-ionomer in deep margins compared to composite, such as less dependence on moisture control,37 caries inhibition due to fluoride release38 and inherent affinity to dentine, although with lower bond strength.39
On the other hand, whether RMGIC prevents microleakage at its interfaces with dentine40 and composite41 is questionable. In addition, it appears to be subjected to water sorption and crack formation that may extend to the underlying dentine.42 RMGIC is also less suitable when calcium silicate cements are used in the pulp chamber (for example, perforation repairs or vital pulp therapy) as it achieves a weaker bond to these materials compared to composite.43
Pure calcium silicate cements, such as Biodentine (Septodont, France), have also been used for the open-sandwich technique in combination with overlying composite build-up, especially in vital pulp therapy cases.44 However, more long-term data would be necessary due to their low mechanical properties and bond to dentine that is considerably inferior to composite and requires a seven-day maturation to become at least comparable to glass-ionomer.45
Taking the above into consideration and despite their decreased technique-sensitivity, open-sandwich approaches do not appear to offer any significant benefit over composite techniques for pre-endodontic restoration.
Periodontal implications
A common concern regarding restorative techniques is the potential impact on periodontal tissues. When not impinging on STA, well-fitted subgingival composite restorations can conform with periodontal health and clinical attachment gain in patients with healthy periodontium and stringent oral hygiene.46 When infringing within the STA, composite CMR is reported to induce higher bleeding on probing after 12 months;47 however, when provided under flap (to eliminate the technique-sensitivity of producing a well-fitted restoration at deeply subgingival margins), it appears to result in comparable six-month tissue response to supragingival restorations placed after surgical crown lengthening (SCL).48 Nevertheless, more long-term data would be needed as degradation of CMR composite may take place over time, especially after three years.49 Also, placing subgingival restorations under flap still requires a surgical procedure not much different from that of conventional crown lengthening along with its potential drawbacks such as gingival recession.50
Surgical/orthodontic techniques
Restorative techniques may be limited in certain clinical situations (Fig. 1), especially when:
-
Ferrule effect needs to be enhanced
-
STA violation is expected
-
Isolation of the cavity is not possible (for example, gingival ingrowth into cavity).
Techniques that can expose tooth tissue may be employed in such cases, either alone or in combination with a restorative build-up (Fig. 3).
Surgical crown lengthening
This approach involves either an apically positioned flap (APF) (with or without osseous resection) or a flapless gingivectomy procedure aiming to expose more tooth tissue in structurally compromised teeth.
Gingivectomy may generally result in less post-operative morbidity than flap surgery,51 and is indicated when there is sufficient width of keratinised tissues (≥3 mm)22 and no STA violation is expected.52 A suitable example would be a case of altered passive eruption, where gingival margin is coronally placed over enamel.53 Techniques to perform gingivectomy include scalpel, electrosurgery and lasers (Nd:YAG, CO2, diode). Scalpel is considered as the 'standard treatment', and although more cost-effective, it is often associated with peri-operative haemorrhage;51 thus, it may complicate isolation for the endodontic treatment to be performed at the same visit. In comparison with scalpel technique, electrosurgery is advantageous in terms of haemostasis, incisional time and post-operative discomfort,54 although when inappropriately performed, it may result in delayed healing and tissue necrosis.55 Lasers have comparable advantages with electrosurgery regarding bleeding control, ease of use and post-operative pain,56 and are generally superior to scalpel in terms of incision accuracy, sterilisation of the surgical field, patient tolerance, tissue rebound and scarring,51 , 57 but they are costly and might cause collateral thermal damage.51
APF is indicated when there is insufficient width of keratinised tissues (<3 mm)22 and/or osseous resection is required to re-establish STA apico-coronal dimension.52 This approach may be necessary in altered active eruption cases, where cementoenamel junction coincides with crestal level.53 Nevertheless, significant tissue rebound is expected, especially within 3-6 months post-surgery,58 , 59 and appears to be associated with several factors, such as thick gingival phenotype, amount of bone removal and flap positioning at crestal level.58 The extended healing time could delay the provision of definitive restoration, jeopardising the outcome of endodontic treatment.60 SCL with bone removal may also result in more than a twofold risk of extraction of endodontically treated posterior teeth after ten years,61 potentially due to the negative impact on crown-to-root ratio61 and furcation exposure.62 Long-term clinical studies indicate that approximately half of endodontically treated teeth with osseous resective SCL will be lost after 10-13 years.61 , 63
In addition, as bone removal often extends to a wider area to prevent disharmony in soft tissue contours, it affects adjacent and non-adjacent sites, causing long clinical crowns, black triangles and papillae loss.50 Consequently, SCL with bone resection is usually not recommended in the aesthetic zone and alternatives, such as orthodontic or surgical extrusion, may be considered instead.
Orthodontic extrusion
Orthodontic extrusion is often preferable to SCL, principally in the aesthetic zone, as it is more conservative, averts bone resection, and secures the root contours and periodontal integrity of the treated and adjacent teeth,50 , 64 while it is highly indicated in patients whose medical condition precludes surgical approaches.65
This technique induces coronal migration of the supporting bone and soft tissues, especially when performed under low-intensity forces (slow extrusion), which may be desirable in certain cases (angular bony defects, lack of keratinised tissues),66 but may also cause aesthetic problems that require secondary surgical correction.67 Nevertheless, this can be avoided with combined supracrestal fibrotomy during the extrusion period.68 Rapid extrusion (with strong traction forces) results in less coronal displacement of periodontal tissues,69 but requires an extended retention period and is associated with a higher occurrence of ankylosis67 and root resorption.70
Orthodontic extrusion is generally contraindicated in cases of short roots, ankylosis, hypercementosis, furcation exposure, root proximity and premature closure of embrasures.71 Further limitations of this method include long treatment duration, patient compliance, unfavourable aesthetics, high cost, availability of proper anchorage, impairment of oral hygiene and risk of relapse.71 , 72
Surgical extrusion
Surgical extrusion involves the intentional coronal displacement of the remaining tooth structure within the socket, with or without rotation. Rotation may be employed in order to shift subgingival fracture lines to a more favourable position, limiting the amount of extrusion required, as well as to increase cervical width and avoid unwanted black triangles due to the narrower root diameter of extruded teeth.73 , 74
Unlike orthodontic extrusion, this technique is typically not applicable to molars75 but is reported to produce comparable results with regards to periodontal healing,76 marginal bone loss and root resorption.77 It also consists of a simple one-step procedure, which encourages patients' cooperation and minimises treatment time and cost,73 , 74 as well as maintaining gingival architecture.78 Additionally, no cases of ankylosis concerning surgically extruded teeth have been described in the literature73 , 74 , 78 , 79 and short-term non-rigid splinting may be an additional preventive measure.74
Contraindications include anatomical variations (such as hypercementosis), inadequate root length and divergent or thin roots.75 , 79 Surface (non-progressive) root resorption is the most frequent complication (30%) while progressive root resorption is rare (3.3%) and it had mostly been associated with earlier flap approaches which included luxation forces to the apex.74 Less traumatic techniques using periotomes78 or a vertical extraction system79 limit the risk of resorption, although the former may still transfer lateral forces to the socket,75 while the latter may risk perforation as it works via a self-tapping screw anchored into the root canal.79 Other complications of surgical extrusion include slight mobility and marginal bone loss, which both seem to be more associated with premolars,79 , 80 while the incidence of tooth loss is low (5%).74
In the literature, it is often suggested to fill root canals of teeth during surgical or orthodontic extrusion with calcium hydroxide71 , 74 , 78 in order to prevent resorption activity due to its antibacterial and healing properties. This might be applicable in cases where initiation of endodontic treatment is urgent; however, concerns arise regarding the ability to achieve adequate isolation.81 Endodontic treatment can be completed after splint removal or during the healing phase as long as splinting type and location allow proper access and placement of the rubber dam.75
Conclusion
It is evident that pre-endodontic restoration has many advantages for the predictability of endodontic treatment for structurally compromised teeth and clinicians have a plethora of techniques to employ. Considering that high-quality evidence in this field is still limited, future controlled studies comparing the effect of available methods on the outcomes of endodontic treatment would be highly recommended.
References
- 1.
European Society of Endodontology. Quality guidelines for endodontic treatment: consensus report of the European Society of Endodontology. Int Endod J 2006; 39: 921-930.
- 2.
Tanikonda R. Canal projection using gutta-percha points: A novel technique for pre-endodontic buildup of grossly destructed tooth. J Conserv Dent 2016; 19: 194-197.
- 3.
Rao S, Ballal N V. Endodontic Buildups - A Case Series. J Dentists 2017; 5: 6-12.
- 4.
Naoum H J, Chandler N P. Temporization for endodontics. Int Endod J 2002; 35: 964-978.
- 5.
ElAyouti A, Serry M I, Geis-Gerstorfer J, Löst C. Influence of cusp coverage on the fracture resistance of premolars with endodontic access cavities. Int Endod J 2011; 44: 543-549.
- 6.
Pane E S, Palamara J E, Messer H H. Stainless steel bands in endodontics: effects on cuspal flexure and fracture resistance. Int Endod J 2002; 35: 467-471.
- 7.
Gingell J C, Zeller G G, Whitaker G C. Potential hazards of copper band utilization: two case reports. Gen Dent 1982; 30: 500.
- 8.
Brady W F. Composite resin interim restorations for broken-down nonvital posterior teeth. J Am Dent Assoc 1983; 106: 462-466.
- 9.
Dawood A, Patel S. The Dental Practicality Index - assessing the restorability of teeth. Br Dent J 2017; 222: 755-758.
- 10.
McDonald A, Setchell D. Developing a tooth restorability index. Dent Update 2005; 32: 343-344, 346-348.
- 11.
Abbott P V. Assessing restored teeth with pulp and periapical diseases for the presence of cracks, caries and marginal breakdown. Aust Dent J 2004; 49: 33-39; quiz 45.
- 12.
Naumann M, Schmitter M, Frankenberger R, Krastl G. "Ferrule Comes First. Post Is Second!" Fake News and Alternative Facts? A Systematic Review. J Endod 2018; 44: 212-219.
- 13.
Dietschi D, Duc O, Krejci I, Sadan A. Biomechanical considerations for the restoration of endodontically treated teeth: a systematic review of the literature-Part 1. Composition and micro-and macrostructure alterations. Quintessence Int 2007; 38: 733-743.
- 14.
Plotino G, Grande N M, Isufi A et al. Fracture Strength of Endodontically Treated Teeth with Different Access Cavity Designs. J Endod 2017; 43: 995-1000.
- 15.
Jepsen S, Caton J G, Albandar J M et al. Periodontal manifestations of systemic diseases and developmental and acquired conditions: Consensus report of workgroup 3 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol 2018; 89: S237-S248.
- 16.
Schmidt J C, Sahrmann P, Weiger R, Schmidlin P R, Walter C. Biologic width dimensions - a systematic review. J Clin Periodontol 2013; 40: 493-504.
- 17.
Perez J R, Smukler H, Nunn M E. Clinical evaluation of the supraosseous gingivae before and after crown lengthening. J Periodontol 2007; 78: 1023-1030.
- 18.
van der Velden U. Probing force and the relationship of the probe tip to the periodontal tissues. J Clin Periodontol 1979; 6: 106-114.
- 19.
Armitage G C. Manual periodontal probing in supportive periodontal treatment. Periodontol 2000 1996; 12: 33-39.
- 20.
Arora R, Narula S C, Sharma R K, Tewari S. Evaluation of supracrestal gingival tissue after surgical crown lengthening: a 6-month clinical study. J Periodontol 2013; 84: 934-940.
- 21.
Grossmann Y, Sadan A. The prosthodontic concept of crown-to-root ratio: a review of the literature. J Prosthet Dent 2005; 93: 559-562.
- 22.
Maynard Jr J G, Wilson R D. Physiologic dimensions of the periodontium significant to the restorative dentist. J Periodontol 1979; 50: 170-174.
- 23.
Dietschi D, Spreafico R. Current clinical concepts for adhesive cementation of tooth-coloured posterior restorations. Pract Periodontics Aesthet Dent 1998; 10: 47-54; quiz 56.
- 24.
Magne P, Spreafico R C. Deep Margin Elevation: A Paradigm Shift. Am J Esthet Dent 2012; 2: 86-96.
- 25.
Roggendorf M J, Krämer N, Dippold C et al. Effect of proximal box elevation with resin composite on marginal quality of resin composite inlays in vitro. J Dent 2012; 40: 1068-1073.
- 26.
Magne P, Kim T H, Cascione D, Donovan T E. Immediate dentin sealing improves bond strength of indirect restorations. J Prosthet Dent 2005; 94: 511-519.
- 27.
Köken S, Juloski J, Sorrentino R, Grandini S, Ferrari M. Marginal sealing of relocated cervical margins of mesio-occluso-distal overlays. J Oral Sci 2018; 60: 460-468.
- 28.
Lopes L C P, Terada R S S, Tsuzuki F M, Giannini M, Hirata R. Heating and preheating of dental restorative materials-a systematic review. Clin Oral Investig 2020; 24: 4225-4235.
- 29.
Dietschi D, Spreafico R. Evidence-based concepts and procedures for bonded inlays and onlays. Part I. Historical perspectives and clinical rationale for a biosubstitutive approach. Int J Esthet Dent 2015; 10: 210-227.
- 30.
Heydrich R W. Pre-endodontic treatment restorations. A modification of the 'donut' technique. J Am Dent Assoc 2005; 136: 641-642.
- 31.
Frese C, Wolff D, Staehle H J. Proximal box elevation with resin composite and the dogma of biological width: clinical R2-technique and critical review. Oper Dent 2014; 39: 22-31.
- 32.
Deliperi S, Alleman D, Rudo D. Stress-reduced Direct Composites for the Restoration of Structurally Compromised Teeth: Fiber Design According to the "Wallpapering" Technique. Oper Dent 2017; 42: 233-243.
- 33.
Bhomavat A S, Manjunatha R K, Rao R N, Kidiyoor K H. Endodontic management of badly broken down teeth using the canal projection system: two case reports. Int Endod J 2009; 42: 76-83.
- 34.
Velmurugan N, Bhargavi N, Neelima L, Kandaswamy D. Restoration of a vertical tooth fracture and a badly mutilated tooth using canal projection. Indian J Dent Res 2007; 18: 87-89.
- 35.
Patel S, Foschi F, Condon R, Pimentel T, Bhuva B. External cervical resorption: part 2 - management. Int Endod J 2018; 51: 1224-1238.
- 36.
Andersson-Wenckert I E, van Dijken J W, Kieri C. Durability of extensive Class II open-sandwich restorations with a resin-modified glass ionomer cement after 6 years. Am J Dent 2004; 17: 43-50.
- 37.
Shimazu K, Karibe H, Ogata K. Effect of artificial saliva contamination on adhesion of dental restorative materials. Dent Mater J 2014; 33: 545-550.
- 38.
Tantbirojn D, Rusin R P, Bui H T, Mitra S B. Inhibition of dentin demineralization adjacent to a glass-ionomer/composite sandwich restoration. Quintessence Int 2009; 40: 287-294.
- 39.
Korkmaz Y, Gurgan S, Firat E, Nathanson D. Shear bond strength of three different nano-restorative materials to dentin. Oper Dent 2010; 35: 50-57.
- 40.
Sawani S, Arora V, Jaiswal S, Nikhil V. Comparative evaluation of microleakage in Class II restorations using open vs. closed centripetal build-up techniques with different lining materials. J Conserv Dent 2014; 17: 344-348.
- 41.
Francois P, Vennat E, Le Goff S, Ruscassier N, Attal J P, Dursun E. Shear bond strength and interface analysis between a resin composite and a recent high-viscous glass ionomer cement bonded with various adhesive systems. Clin Oral Investig 2019; 23: 2599-2608.
- 42.
Czarnecka B, Kruszelnicki A, Kao A, Strykowska M, Nicholson J W. Adhesion of resin-modified glass-ionomer cements may affect the integrity of tooth structure in the open sandwich technique. Dent Mater 2014; DOI: 10.1016/j.dental.2014.05.008.
- 43.
Cantekin K, Avci S. Evaluation of shear bond strength of two resin-based composites and glass ionomer cement to pure tricalcium silicate-based cement (Biodentine). J Appl Oral Sci 2014; 22: 302-306.
- 44.
Koubi G, Colon P, Franquin J C et al. Clinical evaluation of the performance and safety of a new dentine substitute, Biodentine, in the restoration of posterior teeth - a prospective study. Clin Oral Investig 2013; 17: 243-249.
- 45.
Kaup M, Dammann C H, Schäfer E, Dammaschke T. Shear bond strength of Biodentine, ProRoot MTA, glass ionomer cement and composite resin on human dentine ex vivo. Head Face Med 2015; 11: 14.
- 46.
Bertoldi C, Monari E, Cortellini P et al. Clinical and histological reaction of periodontal tissues to subgingival resin composite restorations. Clin Oral Investig 2020; 24: 1001-1011.
- 47.
Ferrari M, Koken S, Grandini S, Ferrari Cagidiaco E, Joda T, Discepoli N. Influence of cervical margin relocation (CMR) on periodontal health: 12-month results of a controlled trial. J Dent 2018; 69: 70-76.
- 48.
Oppermann R V, Gomes S C, Cavagni J, Cayana E G, Conceição E N. Response to Proximal Restorations Placed Either Subgingivally or Following Crown Lengthening in Patients with No History of Periodontal Disease. Int J Periodontics Restorative Dent 2016; 36: 117-124.
- 49.
Bresser R A, Gerdolle D, van den Heijkant I A, Sluiter-Pouwels L M A, Cune M S, Gresnigt M M M. Up to 12 years clinical evaluation of 197 partial indirect restorations with deep margin elevation in the posterior region. J Dent 2019; 91: 103227.
- 50.
Nobre C M, de Barros Pascoal A L, Albuquerque Souza E et al. A systematic review and meta-analysis on the effects of crown lengthening on adjacent and non-adjacent sites. Clin Oral Investig 2017; 21: 7-16.
- 51.
Mavrogiannis M, Ellis J S, Seymour R A, Thomason J M. The efficacy of three different surgical techniques in the management of drug-induced gingival overgrowth. J Clin Periodontol 2006; 33: 677-682.
- 52.
Padbury Jr A, Eber R, Wang H L. Interactions between the gingiva and the margin of restorations. J Clin Periodontol 2003; 30: 379-385.
- 53.
Ragghianti Zangrando M S, Veronesi G F, Cardoso M V et al. Altered Active and Passive Eruption: A Modified Classification. Clin Adv Periodontics 2017; 7: 51-56.
- 54.
Ismail A, Abushouk A I, Elmaraezy A et al. Cutting electrocautery versus scalpel for surgical incisions: a systematic review and meta-analysis. J Surg Res 2017; 220: 147-163.
- 55.
Liboon J, Funkhouser W, Terris D J. A comparison of mucosal incisions made by scalpel, CO2 laser, electrocautery, and constant-voltage electrocautery. Otolaryngol Head Neck Surg 1997; 116: 379-385.
- 56.
Kumar P, Rattan V, Rai S. Comparative evaluation of healing after gingivectomy with electrocautery and laser. J Oral Biol Craniofac Res 2015; 5: 69-74.
- 57.
Pick R M, Colvard M D. Current status of lasers in soft tissue dental surgery. J Periodontol 1993; 64: 589-602.
- 58.
Pilalas I, Tsalikis L, Tatakis D N. Pre-restorative crown lengthening surgery outcomes: a systematic review. J Clin Periodontol 2016; 43: 1094-1108.
- 59.
Al-Sowygh Z H. Does Surgical Crown Lengthening Procedure Produce Stable Clinical Outcomes for Restorative Treatment? A Meta-Analysis. J Prosthodont 2019; DOI: 10.1111/jopr.12909.
- 60.
Ng Y L, Mann V, Gulabivala K. A prospective study of the factors affecting outcomes of non-surgical root canal treatment: part 2: tooth survival. Int Endod J 2011; 44: 610-625.
- 61.
Patil K, Khalighinejad N, El-Refai N, Williams K, Mickel A. The Effect of Crown Lengthening on the Outcome of Endodontically Treated Posterior Teeth: 10-year Survival Analysis. J Endod 2019; 45: 696-700.
- 62.
Dibart S, Capri D, Kachouh I, Van Dyke T, Nunn M E. Crown lengthening in mandibular molars: a 5-year retrospective radiographic analysis. J Periodontol 2003; 74: 815-821.
- 63.
Moghaddam A S, Radafshar G, Taramsari M, Darabi F. Long-term survival rate of teeth receiving multidisciplinary endodontic, periodontal and prosthodontic treatments. J Oral Rehabil 2014; 41: 236-242.
- 64.
Faria L P, Almeida M M, Amaral M F, Pellizzer E P, Okamoto R, Mendonça M R. Orthodontic Extrusion as Treatment Option for Crown-Root Fracture: Literature Review with Systematic Criteria. J Contemp Dent Pract 2015; 16: 758-762.
- 65.
Buskin R, Castellon P, Hochstedler J L. Orthodontic extrusion and orthodontic extraction in preprosthetic treatment using implant therapy. Pract Periodontics Aesthet Dent 2000; 12: 213-219; quiz 220.
- 66.
Ingber J S. Forced eruption. I. A method of treating isolated one and two wall infrabony osseous defects-rationale and case report. J Periodontol 1974; 45: 199-206.
- 67.
Oesterle L J, Wood L W. Raising the root. A look at orthodontic extrusion. J Am Dent Assoc 1991; 122: 193-198.
- 68.
Carvalho C V, Bauer F P, Romito G A, Pannuti C M, De Micheli G. Orthodontic extrusion with or without circumferential supracrestal fibreotomy and root planing. Int J Periodontics Restorative Dent 2006; 26: 87-93.
- 69.
Sabri R. L'allongement coronaire par l'égression orthodontique. Principes et techniques. J Parodontol 1989; 8: 197-204.
- 70.
Minsk L. Orthodontic tooth extrusion as an adjunct to periodontal therapy. Compend Contin Educ Dent 2000; 21: 768-770, 772, 774 passim.
- 71.
Bach N, Baylard J F, Voyer R. Orthodontic extrusion: periodontal considerations and applications. J Can Dent Assoc 2004; 70: 775-780.
- 72.
Smidt A, Gleitman J, Dekel M S. Forced eruption of a solitary nonrestorable tooth using mini-implants as anchorage: rationale and technique. Int J Prosthodont 2009; 22: 441-446.
- 73.
Das B, Muthu M S. Surgical extrusion as a treatment option for crown-root fracture in permanent anterior teeth: a systematic review. Dent Traumatol 2013; 29: 423-431.
- 74.
Elkhadem A, Mickan S, Richards D. Adverse events of surgical extrusion in treatment for crown-root and cervical root fractures: a systematic review of case series/reports. Dent Traumatol 2014; 30: 1-14.
- 75.
Dietrich T, Krug R, Krastl G, Tomson P L. Restoring the unrestorable! Developing coronal tooth tissue with a minimally invasive surgical extrusion technique. Br Dent J 2019; 226: 789-793.
- 76.
Kim S H, Tramontina V A, Ramos C M, Prado A M, Passanezi E, Greghi S L. Experimental surgical and orthodontic extrusion of teeth in dogs. Int J Periodontics Restorative Dent 2009; 29: 435-443.
- 77.
Costa L A, Ribeiro C C, Cantanhede L M, Santiago Júnior J F, de Mendonça M R, Pereira A L. Treatments for intrusive luxation in permanent teeth: a systematic review and meta-analysis. Int J Oral Maxillofac Surg 2017; 46: 214-229.
- 78.
Pham H T, Nguyen P A, Pham T A V. Periodontal status of anterior teeth following clinical crown lengthening by minimally traumatic controlled surgical extrusion. Dent Traumatol 2018; 34: 455-463.
- 79.
Krug R, Connert T, Soliman S, Syfrig B, Dietrich T, Krastl G. Surgical extrusion with an atraumatic extraction system: A clinical study. J Prosthet Dent 2018; 120: 879-885.
- 80.
Choi Y H, Lee H J. Surgical extrusion of a maxillary premolar after orthodontic extrusion: a retrospective study. J Korean Assoc Oral Maxillofac Surg 2019; 45: 254-259.
- 81.
Warfvinge J, Kahnberg K E. Intraalveolar transplantation of teeth. IV. Endodontic considerations. Swed Dent J 1989; 13: 229-233.
Download references
Ethics declarations
The authors declare no conflicts of interest.
Rights and permissions
Open Access. This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0.© The Author(s) 2021
Reprints and Permissions
About this article
Cite this article
Gavriil, D., Kakka, A., Myers, P. et al. Pre-endodontic restoration of structurally compromised teeth: current concepts. Br Dent J 231, 343–349 (2021). https://doi.org/10.1038/s41415-021-3467-0
Download citation
-
Received:
-
Accepted:
-
Published:
-
Issue Date:
-
DOI : https://doi.org/10.1038/s41415-021-3467-0
How to Fix System Thermal Solution Compromised
Source: https://www.nature.com/articles/s41415-021-3467-0?proof=t